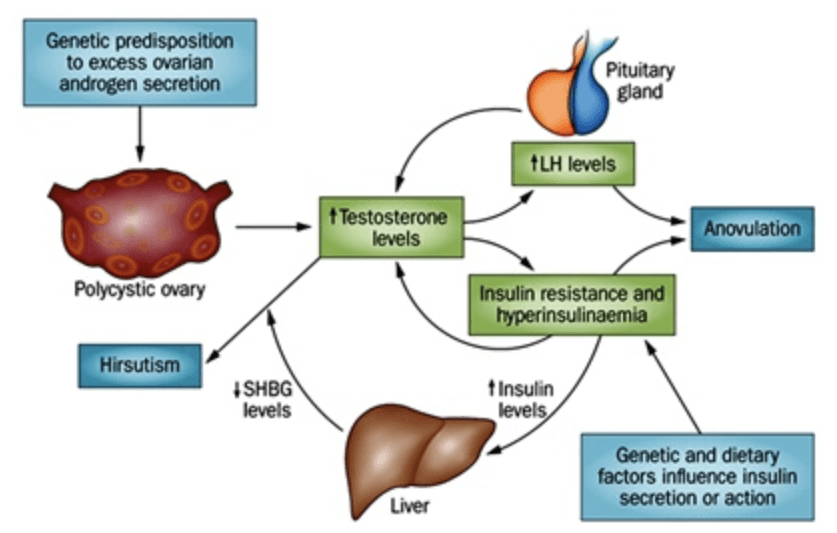
Insulin resistance is a key issue for women with PCOS. This is due to the interplay between high male (androgenic) hormones in a female body. The exact mechanisms are not known, but all women with PCOS need to be evaluated and treated for insulin resistance. If you are worried about your blood sugars, and are a male or a female without PCOS, please continue reading. There is a wealth of information to help you here too!
Let me explain insulin resistance to you simply. Most cells in the body have a lock (receptor) that needs to be opened up by a key (hormone, such as insulin) in order to let glucose into the cell to feed it. Imagine that the lock in a “normal” shaped cell is a square. There is a specific key that fits that lock, also in the shape of the square – insulin is the same square key that matches the lock. When the insulin (key) attaches to the lock on the cell, it opens up and allows glucose into the cell. In a healthy body, the system works well. When we have a free flowing amount of insulin from the pancreas, we have a stable amount of blood sugar in our system. Insulin regulates how much sugar we take in from our diet and use in the cells.
When there is a healthy and balanced diet, along with regular movement and stress management techniques; the blood sugar is likely in good balance. Some people have a genetic predisposition to having blood sugar imbalances in spite of doing everything right. Others, however, eat too much sugar, drink too much alcohol, do not exercise enough, and have unmanaged stress. What happens in this second scenario, is that excess sugar and excess insulin will get stored as triglycerides and often as abdominal fat. This extra fat around the waste is difficult to lose because of the vicious cycle of insulin resistance.
Let us go back to the cell, the lock and key analogy. Now we have a cell that has gotten bigger because of gaining weight. When the cell gets bigger, the lock gets bigger too. The problem is that the key (the insulin) does not change shape. In order to get the now bigger cell to unlock (the lock is now a rectangle), it requires 2, 3, or even 10 keys (insulin squares to match the new rectangle lock) depending on the new size of the cell or how resistant it is. With excess insulin and glucose floating around in the blood trying to get the cells to open up, we store more triglycerides, creating more fat and also more of the symptoms that people feel from insulin resistance.
Brain fog, fatigue, sugar and carbohydrate cravings, increased hunger and thirst, increased urination, tingling in toes and feet are all common signs of insulin resistance.
What can you do if you have insulin resistance? Focus on getting in 80 grams of protein throughout the day, eating healthy fats (like olive oil, nuts, seeds, and avocados), and incorporating 8 servings of fruits and vegetables a day. Ideally aim for two times the vegetables as fruit and note that high starch veggies are quickly metabolized into sugar too. So don’t eat too many starchy veggies like corn and potatoes to name a few. Incorporating daily movement as well as finding ways to reduce your stress will make a world of difference as well.
When you go to the doctor’s office with blood sugar concerns, you can expect your doctor to order some labs for you. We will make sure your labs are complete with cholesterol, blood sugar and a complete metabolic panel, insulin, and hemoglobin A1c. If stress is a significant part of your blood sugar picture, we will likely recommend testing your adrenals so that we have an idea of how your reserves are holding up.
For treatment options we have a large selection of herbs, natural remedies, nutrition, and mind-body support that will be individualized to wherever you are with your blood sugar regulating needs. If medication is important for your care, we often will prescribe metformin, which is a medication used to sensitize your cells to insulin. Many people with diabetes as well as people who have PCOS safely use this medication.
Please let us know how we can support you in your wellness, we are here for you!
Image Credit: http://waocp.com/